There is an increasing need to deliver high value care.1 High value maternity care will produce the highest level of benefit for women at a given cost,2 and deliver what matters the most to women. However, to move beyond traditional narrow and passive measurement of value, there is a need to partner with stakeholders to identify priorities for change, identify evidence for how to achieve this change, integrate measurement activities, and promote effective implementation, in a continuous, learning cycle – a Learning Health System (LHS). The LHS is an approach to healthcare provision that integrates community, researchers and clinical practice with the ultimate goal of quality improvement in healthcare for better health outcomes. But to date there are only a handful of examples of LHS, with none in maternity care.3 A robust Framework for implementing a LHS has been codeveloped, which could be applied in maternity care.4
The LHS Framework
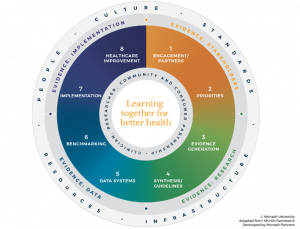
A LHS approach can be implemented through a new Framework that outlines a robust, codeveloped process. Specifically, this framework was co-produced with all relevant stakeholders, with a diverse steering committee (including community), a systematic review of effective LHS models,3 extensive qualitative interviews, and coproduction workshops.5 The LHS Framework (Figure 1) has four fundamental pillars to facilitate the LHS process:
- evidence from stakeholders (including Patient Reported Experience Measures and Patient Reported Outcome Measures)
- evidence from research (including evidence based practice)
- evidence from routine data on healthcare performance
- evidence from implementation and improvement to meet stakeholder and community priorities
Figure 1: The Learning Health System Framework
Next steps
Importantly, this iterative system, centralised around the principle of all stakeholders, including women, learning together for better health, presents an evidence-based system level approach to embed routine measurement of value as determined by women. In short, this approach is critical in the delivery of women-focused, high-quality, sustainable maternal health care. Likewise, it is essential for high value maternity care. This LHS framework will be implemented across healthcare service areas, including in maternity care.
Highlighted article
Enticott, J.C., Melder, A., Johnson, A., Jones, A., Shaw, T., Keech, W., et al. (2021). A Learning health system framework to operationalise health data to improve quality care: an Australian perspective. Frontiers in Medicine, 1824.
Blog written by
Associate Professor Emily Callander, Monash Centre for Health Research and Implementation, Monash University.
References
- Braithwaite, J., Glasziou, P., Westbrook, J. (2020). The three numbers you need to know about healthcare: the 60-30-10 challenge. BMC Medicine, 18, 1-8.
- von Gruenigen VE, Powell DM, Sorboro S, McCarroll ML, Kim U. (2013). The financial performance of labor and delivery units. American Journal of Obstetrics and Gynecology, 209(1), 17-19.
- Enticott, J,, Johnson, A., Teede, H. (2021). Learning health systems using data to drive healthcare improvement and impact: a systematic review. BMC Health Services Research, 21(1), 1-16.
- Enticott, J.C., Melder, A., Johnson, A., Jones, A., Shaw, T., Keech, W., et al. (2021). A Learning health system framework to operationalise health data to improve quality care: an Australian perspective. Frontiers in Medicine, 1824.
- Enticott, J., Braaf, S., Jones, A., Johnson. A., Teede, H. (2020). Leaders’ perspectives on learning health systems: a qualitative study. BMC Health Services Research, 20(1), 1-13.